Can Histamine Cause Anxiety?
TL:DR: Histamine acts to upregulate the body’s defences; it makes you more alert, and sometimes hyper-alert, and puts the body and nervous system ready to respond to injury. That is why an increase of histamine in the body causes a sense of anxiety, even to the extent of creating a panic attack.
There are ways of reducing the amount of histamine in the body. For that, please read on.
Histamine is a biological substance that is chemically classified as an amine, an organic molecule with an ammonia-like structure (NH3). Histamine-metabolizing enzyme genetic polymorphism is responsible for variability variation in histamine metabolism and is linked to a variety of illnesses.
This means that because of your genetic inheritance, this polymorphism may mean you are more sensitive to histamine, and show more allergies probably, than someone else.
Histamine is a neurotransmitter that plays an important role in the body’s immune system and blood pressure levels. It’s also responsible for regulating stomach acid levels, as well as controlling blood sugar levels and levels of alertness.
However, histamine can also play a role in causing anxiety, especially in people who have histamine intolerance.
In this article, we’ll discuss the role of histamine in anxiety and discuss some ways it can affect anxiety levels. We’ll also provide tips on how to test for histamine intolerance and how to treat it if you’re diagnosed. So whether you’re suffering from reactive anxiety or chronic anxiety, make sure to read on to learn more about histamine and its role in anxiety!
Histamine
Histamine was discovered in 1910 and since then, it has been known that it is a key neurotransmitter, alongside others like GABA, serotonin and dopamine. Histamine sends messages between nerve cells in the brain, spinal cord, and uterus.
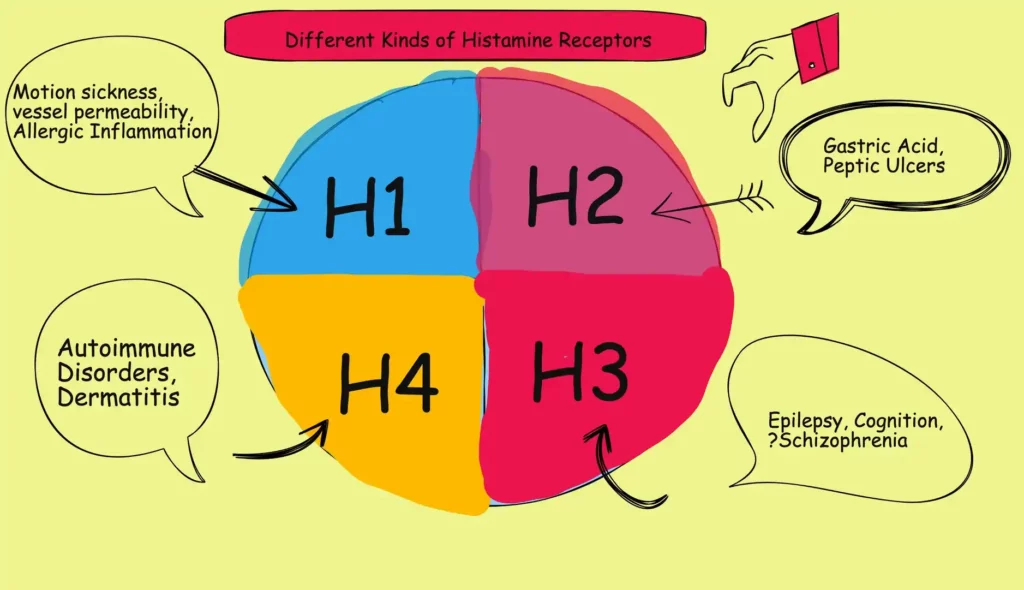
The body has four types of histamine receptors, known as H1R, H2R, H3R, and H4R.
H1R stimulates neurons in the brain and regulates the sleep-wake cycle. Because histamine activates these receptors, insomnia is one of the most prevalent symptoms of histamine intolerance, and antihistamines that act on them create a sedative effect.
These receptors are also known to activate the body’s danger response, causing noradrenalin (norepinephrine) to be released into the bloodstream, which results in a feeling of anxiety.
H2R is excitatory, like H1R, but it primarily affects perception, memory, learning, reward, pleasure, and pain
H3R blocks neurons from producing histamine. These histamine receptors are also in charge of controlling the release of other neurotransmitters in the brain.
Most of the histamine in the body is made in granules in mast cells and white blood cells called basophils.
In the immune response, it makes the capillaries more open to white blood cells and some proteins, so they can reach pathogens in infected tissues. Histamine is a key part of itching and is involved in the inflammatory response.
Mast cells are most common in places that could get hurt, like the nose, mouth, and feet, as well as on the inside of the body and in blood vessels. They are there to release vast amounts of histamine on injury.
Some drugs, like morphine, can increase the supply of histamine out and let it out into the body.
Even though histamine is small compared to other biological molecules (it only has 17 atoms), it is very important to the body. It plays a role in 23 different functions in the body.
It causes nitric oxide and other compounds that relax smooth muscle cells in blood vessels to be made and released. This causes veins and capillaries.
immune response to widen, and thus drop blood pressure. We have long known that blood pressure drops when histamine is injected into a vein.
When the permeability of the blood vessels goes up, fluid leaks out of the capillaries and into the tissues. This causes the classic signs of an allergic reaction. An allergic response might include a runny nose and watery eyes, and general flushing and redness.
Histamine stimulates vasodilation, and increases vascular permeability, heart rate, cardiac contraction, and glandular secretion. This explains its key role in anaphylactic shock.
Histamine does not cross the brain blood barrier and so the brain makes its own histamine in specialist cells.
Histamine producing neurons in the brain fire quickly when you are awake, more slowly when you are relaxed or tired, and don’t fire at all during REM and NREM sleep.
They are therefore intimately associated with levels of alertness, and the highest level of alertness is anxiety when the person is primed to look out for threat. As well as priming your body for danger and hurt, it also activates the mind to do the same, and this feels like anxiety.
Histamine also stimulates the adrenal glands’ secretion of adrenalin (also known as epinephrine) and noradrenaline (also known as norepinephrine). Many of the physical symptoms of anxiety are caused by an increase in these hormones, including heart palpitations, shortness of breath, sweating, shaking, and nausea.
Why Might You Have Too Much Histamine In Your System?
Do You Have Mastocytosis?
Mastocytosis is an uncommon condition with unknown incidence rates. According to one study, one in every 10,000 people in the United States had this condition. Mastocytosis affects both men and women in equal proportions. The condition can start in childhood or in maturity.
Mastocytosis is a rare disease in which mast cells grow in number and overproduce histamine.
This is a very rare condition. However, if you may choose to contact your healthcare provider to rule it out.
Do You Have Histamine Intolerance?
Histamine intolerance is a condition in which people are sensitive to histamine-containing foods and medications.
Histamine intolerance can cause trouble sleeping, rapid heartbeat with pounding heart, shortness of breath, feeling sick, and sweating. Some other common symptoms of histamine intolerance include anxiety, fatigue, and headaches.
If you’re histamine intolerant, following a histamine free diet, taking histamine busting supplements (DAO in the main) or taking antihistamines may help relieve symptoms, including high-levels of anxiety.
Do You Have Estrogen Related Elevated Histamine?
Many women complain of anxiety levels increasing in line with their monthly cycle. We also see women in peri-menopausal or menopausal stages complaining of inability to sleep, increased anxiety and other physical symptoms that might be related to higher levels of histamine.
There are two ways in which estrogen and histamine affect each other:
Increased histamine can cause estrogen levels to go up (think heavy periods, endometriosis, migraines). So if you have an inflammation response in your body, you may produce increased oestrogen.
It is critical to understand that histamine released by the body stimulates the ovaries to create more estrogen. This rise in estrogen raises histamine produced by cells in the brain.
And this can be a vicious cycle, because increased estrogen makes mast cells release more histamine, and that can increase feelings of anxiety.
Do You Have Small Intestinal Bacterial Overgrowth?
SIBO is an acronym for “small intestinal bacterial overgrowth.” It’s a condition in which the amount of bacteria in the small intestine exceeds normal levels. This can cause problems with digestion and absorption, as well as inflammation and gas accumulation.
People with this condition often experience bloating, abdominal pain, nausea, diarrhea, fatigue, and headache. They may also have an increased risk of other diseases, such as Crohn’s disease or food allergies.
There is no known cure for SIBO, but treatment usually involves antibiotics to kill off the excess bacteria and lifestyle changes (such as eating probiotics) to restore balance in the gut flora. If left untreated, it can lead to serious health complications such as malnutrition or even chronic pain syndromes unrelated to gut health issues.
There are many causes of SIBO and histamine intolerance – genetic factors play a role in about 30% of cases, while environmental factors contribute to 40%. The major culprits behind both conditions are grains and dairy products. Both foods contain high levels of gluten and casein (two proteins found in these foods), which trigger the body into over-reacting.
This leads to the formation of inflammation in the intestines – essentially ‘flooding’ them with too much bacteria and yeast.
We know histamines are part of this inflammatory response.
If you’re histamine intolerant, it’s important to keep your gut healthy by eating a balanced diet and supplementing with probiotics. Additionally, you should avoid histamine-rich foods like red meat, eggs, milk, and cheese.
L-histidine and anxiety
The body makes the neurotransmitter histamine from the amino acid L-histidine. Our body can not make this essential substance and so we get it from our food, or from supplements, or we can absorb it from certain cosmetics.
However, some health professionals suspect that certain individuals are histamine intolerant, and when they consume even normal levels of l-histidine from their food, they produce to much histamine and then suffer the symptoms described above.
You must not cut out l-histidine altogether, as it is an essential amino acid. A Japanse study in 2014, admittedly in mice, showed that low intake of l-histidine created anxiety behaviour in the animals.
https://academic.oup.com/jn/article/144/10/1637/4575123?login=false
Another study here
https://www.sciencedaily.com/releases/2005/03/050328181920.htm
Showed that low histamine levels in the brain caused anxiety.
This seems to suggest that both low and high levels of histamine cause anxiety.
Though this might seem paradoxical, the body always strives for homeostasis — keeping systems at the right levels. Comparably, too much sodium and too little sodium are both harmful. What the body wants is just right.
There are several ways to increase your L-histidine intake without having to eat foods containing histamine or take supplements containing it. One of the most effective ways to do so is by supplementing with L-histidine-rich foods. These foods include poultry, fish, legumes, nuts, and seeds.
Additionally, taking histamine-busting supplements can help to reduce histamine in the body and relieve symptoms of anxiety.
https://academic.oup.com/jn/article/144/10/1637/4575123?login=false
Mast Cell Activation Syndrome
MCAS and Histamine Intolerance are closely related in symptoms and health professionals are in disagreement whether histamine intolerance is a subset of MCAS. Histamine is a critical but possibly harmful mast cell mediator that is involved in the immune system response. When exposed to an allergen, mast cells produce histamine into the surrounding connective tissues. Mast cell histamine operates by increasing blood artery permeability, allowing white blood cells and proteins easier access to damaged tissues.
Low magnesium levels are frequently linked to Mast Cell Activation Syndrome (MCAS) and Histamine Intolerance Without enough magnesium, it’s difficult to regain health.
Magnesium citrate and magnesium sulphate were the two types (Epsom salts). Magnesium citrate can cause itching.
MCAS is a disorder in which the patient has repeated bouts of anaphylactic symptoms such as hives, swelling, low blood pressure, trouble breathing, and severe diarrhoea. During these events, high quantities of mast cell mediators are released.
Mast cell mediator inhibitors or blockers are used to treat the episodes. The episodes are referred to as “idiopathic” since the mechanism is unknown, they are not produced by allergic antibodies or secondary to other known diseases that activate normal mast cells.
Diamine Oxidase
Some people take diamine oxidase to help with histamine intolerance, which can cause headaches, stomach problems, and skin conditions.
Your body makes an enzyme called diamine oxidase (DAO) to break down the histamine in foods.
If your DAO levels are not high enough, and you don’t have enough of this enzyme, you might have histamine intolerance, which is also known as food histaminosis or enteral histaminosis. When you eat foods with histamine, this can make you sick.
It’s important to understand that this does not mean you are allergic to these foods, just that you can’t break down the histamine sufficiently, and it is the high level of histamine that is causing your symptoms.
You can fix this if you can do something to improve how your body breaks down histamine, and so some people take diamine oxidase (DAO) supplements.
Anti Histamines
There are medications called antihistamines. You will not be surprised to learn they were invented to sedate patients.
First-generation H1 antihistamines can cross the blood-brain barrier and make you sleepy by blocking histamine H1 receptors, so less histamine is available and therefore you are less alert, ultimately falling asleep on sufficient doses.
Remember, some histamines are sedating and will make you sleepy, so you should not drive or operate machinery or do anything that requires focus. They can be useful, however, to help you get to sleep.
Examples of sedating antihistamines are:
- Promethazine (Phenegan)
- Diphenhydramine (Nytol,)
- Chlorphenamine (Piriton)
Examples of less-sedating antihistamines
- Fexofenadine
- Loratadine
- Cetirizine
All of these can cause sedation, especially at high doses, just not as much as the sedating anti-histamines.
Side Effects of Antihistamines
Drowsiness, with some as noted above, but also, Antihistamines, and many related psychiatric drugs cause a loss of libido and an inability to get an erection because they block histamine receptors from working properly, and take you from a state of bodily activation to one of sedation.
It should be noted that antihistamines do not have government approved licenses for treating anxiety and can leave you with a drowsiness hangover the next day.
Anticholinergic Burden
Antihistamines are also suppress the cholinergic system. This means their sedating effect can cause negative side-effects in the short and long term.
These can cause adverse events such as disorientation, dizziness, and falls in individuals over the age of 65. These have been linked to an increase in patient mortality.
There is research that shows that long-term use of sedating antihistamines can cause a not insignificant risk of dementia.
We would guess, but it has not been established, that lesser sedating antihistamines pose less of a risk of dementia in the long term.
Low Histamine Foods You Could Eat
Eating mostly low-histamine meals may limit histamine exposure and accumulation in your body. Foods low in histamine include:
- fresh fish and meat and eggs.
- most fresh vegetables — except for spinach, tomatoes, avocado, and eggplant
- most fresh fruit — except for citrus and some berries
- oils such as coconut and olive oil
- grains such as rice, quinoa, corn, teff, millet, and pomegranates
- Foods are high in Vitamin C, quercetin, vitamin B6, omega-3 fatty acids, and riboflavin can help lower histamine production.
While additives like phosphorus are low in histamine and other amines, they can sometimes cause the body’s endogenous histamine to be released and should probably be avoided.
High Histamine Foods You Might Avoid
Another technique for controlling symptoms of histamine intolerance and poor DAO synthesis is to reduce or eliminate foods high in histamine or those that provoke histamine production.
The following foods contain high quantities of histamine and may cause histamine release:
- fermented foods such as sauerkraut, pickles, yoghurt, and kimchi alcoholic beverages such as beer, wine, and liquor shellfish
- Cheeses and smoked and cured meats are examples of dairy aged foods.
- Peanuts and cashews.
- Citrus fruits, bananas, papaya, and strawberries.
- vegetables such as tomatoes, spinach, eggplant, and avocado
- food additives, colorings, and preservatives
- licorice and cacao.
However, because the food options on a low histamine diet can be limited, you may be at risk of nutritional deficiencies.
A Summar of The Ways to Better Manage Anxiety Induced by Excess Histamine
Rule Out SIBO
Get checked for Small Intestinal Bacterial Overgrowth (SIBO). Speak to your doctor or other healthcare professional for advice. They may recommend a watchful waiting period, or they may prescribe antibiotics.
Try Diamine Oxidase Supplements (DAO)
If you have excessive histamine because you lack DAO, then it is worth trying for a month to see whether they improve your symptoms and anxiety.
Avoid High Histamine Foods
see list above
Prefer Low Histamine Foods
See list above
Other Supplements
It may be helpful to take Vitamin C, Vitamin B6, Vitamin B12, zinc (Zn) and magnesium (Mg)
Take Over The Counter Antihistamines
But only for short periods.
Rule out Mastocytosis
It is extremely unlikely you have this rare condition.
Conclusion
Histamine is a neurotransmitter that is responsible for the regulation of many bodily functions. In high levels, histamine can cause anxiety and other symptoms, such as heartburn, sneezing, and headaches. If you think that histamine may cause your anxiety, it’s important to consult with a doctor to rule out histamine intolerance. There are various ways to manage anxiety caused by histamine levels that are too high.
I hope you found this helpful.
Related Articles
Top 5 Herbs in Ayurveda for Treatment of OCD
Depression After Stopping Drinking
5 Most Effective Antidepressants for Anxiety and Depression (and 3 you should avoid)
How To Explain Anxiety To Someone